You may say you have the stomach flu if you have diarrhea and vomiting. These symptoms often are due to a condition called gastroenteritis. With gastroenteritis, your stomach and intestines are irritated and inflamed. The cause is typically a viral or bacterial infection.
What is Gastroenteritis?
Gastroenteritis is an inflammation of the lining of the stomach and intestines. There can be many different causes of gastroenteritis:
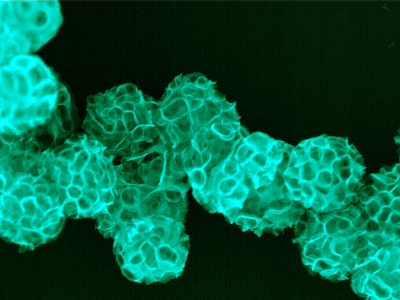
- Viruses
- Bacteria
- Parasites
- Chemicals
- Reactions to certain medicines and food
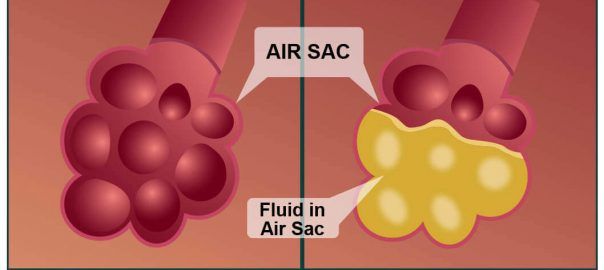
Viral gastroenteritis is the most common type. Many different viruses, including noroviruses and rotaviruses, can cause it. Some people call viral gastroenteritis the stomach flu. But this name needs to be medically correct. Flu viruses do not cause it. The flu is a respiratory infection that affects your nose, throat, and lungs. When gastroenteritis is caused by consuming foods or drinks contaminated with viruses, bacteria, parasites, or chemicals, this is called food poisoning.
The viruses, bacteria, and parasites that cause gastroenteritis can also spread from person to person. You could be infected when you touch something with germs on it and then touch your eyes, mouth, or nose.
What Are The Symptoms Of Gastroenteritis?
The symptoms of gastroenteritis include:
- Nausea
- Vomiting
- Diarrhea
- Pain or cramping in your abdomen
- Sometimes fever
Gastroenteritis is usually not serious. But, it can sometimes cause lead to dehydration or cause severe symptoms. Certain people are at higher risk for these problems. They include:
- Pregnant women
- Older adults
- People with weakened immune systems or other serious health conditions
- Infants
- Babies who were born prematurely or had other health conditions
What Is The Treatment For Gastroenteritis?

There’s often no specific medical treatment for viral gastroenteritis. Antibiotics aren’t effective against viruses. Treatment first involves self-care measures, such as staying hydrated.
To help keep yourself more comfortable and prevent dehydration while you recover, try the following:
- Let your stomach settle. Stop eating solid foods for a few hours.
- Try sucking on ice chips or taking small sips of water often. Consider drinking clear soda, clear broths, or non-caffeinated sports drinks. In some cases, you can try oral rehydration solutions. Drink plenty of liquid every day, taking small, frequent sips.
- Ease back into eating. As you’re able, you can return to eating your normal diet. You might find that you can eat bland, easy-to-digest foods at first, such as soda crackers, soup, oats, noodles, bananas, and rice. Stop eating if your nausea returns.
- Avoid certain foods and substances until you feel better. These include caffeine, alcohol, nicotine, and fatty or highly seasoned foods.
- Get plenty of rest. The illness and dehydration may have made you weak and tired.
- Try anti-diarrhea medications. Some adults may find it helpful to take to manage their symptoms. However, avoid these if you have bloody diarrhea or fever, which could be signs of another condition.
Medication that can be used for the condition:
- Dramamine – is a highly soothing drug that works by helping your body maintain its sense of balance. It belongs to a group of medications called antihistamines.
What Are Serious Cases Of Gastroenteritis?
Older adults or very young children are more vulnerable to the symptoms of gastroenteritis. They’re also at a higher risk of complications. If you have a loved one at a higher risk, keep a close eye on them so they can get medical care if needed.
Complications of these infections include high fevers, muscle pain, and inability to control bowel movements. Some bacterial infections can cause:
- Kidney failure
- Bleeding in your intestinal tract
- Anemia
Quickly seeking treatment for bacterial gastroenteritis lessens your risk of complications. Gastroenteritis should last only a few days and does not normally require treatment. Medication for nausea or diarrhea can be useful for adults but may not be safe for children. Antibiotics are rarely helpful. The most important treatment for gastroenteritis is to drink fluids. Frequent sips are easier for young children than a large amount. Keep regularly drinking even if you are vomiting. You can also buy rehydration fluids from a pharmacy. These are the best fluids to use in gastro cases, especially for children.